Resources
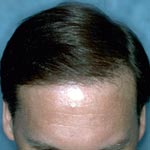
Explore our resources for hair transplant patients.
Everything you want to know about hair loss, hair transplant surgery, forehead reduction hairline lowering, and scalp micropigmentation. The doctors at NHI Medical have spent over two decades innovating in the field of hair loss treatment, receiving dozens of U.S. Patents and publishing many books and articles in the process.